Liver enzymes
 Liver enzymes are proteins that help to speed up a chemical reaction in the liver. Liver function tests are blood tests that are used to evaluate various functions of the liver – for example, metabolism, storage, filtration and excretion, which are often performed by liver enzymes. However, not all liver function tests are measures of enzyme function.
Liver enzymes are proteins that help to speed up a chemical reaction in the liver. Liver function tests are blood tests that are used to evaluate various functions of the liver – for example, metabolism, storage, filtration and excretion, which are often performed by liver enzymes. However, not all liver function tests are measures of enzyme function.
Liver enzymes, which are found in normal plasma or serum, can be divided into different groups.
They are – aspartate aminotransferase (AST or SGOT) and alanine aminotransferase (ALT or SGPT). Together they are known as transaminases. Alkaline phosphatase (AP) and gamma-glutamyl transferase (GGT) – are known as cholestatic liver enzymes. Elevations of these liver enzymes can indicate the presence of liver disease.
Secretory enzymes, synthesizing in the liver, normally allocated in the blood plasma, which play a physiological role, such as enzymes involving in the process of blood clotting (AC globulin), cholinesterase. Any damage to the liver reduces their synthesis and activity of these enzymes decreases.
Aspartate and Alanine aminotransferase (AST and ALT)
Certain enzymes enter into the blood from the tissues, where they perform intracellular functions. Some of them are in the cell cytosol (LDH, ALT, AST), others – in the mitochondria (GGT, AP), etc. Any damage to the liver and enzymes from the cells is washed in the blood, and their activity increases. Greatest diagnostic value is the definition of ALT and AST. Activity of serum transaminases: AST – 5-40 U / L, ALT – 5: -43 U / liter. In acute parenchymatous hepatitis ALT increases to 20-30, sometimes 100 times or more. The activity of AST increases several smaller.
Except liver, AST enzymes are often found in heart, muscle, kidney, and brain, where it is released into serum at the same time one of these tissues is damaged. For instance, with heart attack and muscle disorders rises the AST level in serum. And notice that it is therefore, not a highly specific indicator of liver injury.
Concerning ALT (SGPT), so this one is practically found in the liver. Of course it doesn’t mean that ALT concentrated only in the liver, but as a rule it’s the main place of this enzyme allocation. Thus, as the result of liver injury it is released into the bloodstream and often serves as a fairly specific indicator of liver status.
In order to educe the level of abnormal aminotransferase you should know the main diseases that may cause them.
Commonly the high level of AST and ALT in the liver can easily damage numerous liver cells (extensive hepatic necrosis) and even leads to the cell death. The higher the ALT levels, there are more death cells in the liver. However, ALTs are not always good indications of how well the liver is functioning; only a liver biopsy can reveal that. So, these diseases may cause increased level of AST and ALT liver enzymes: acute viral hepatitis A or B, pronounced liver damage inflicted by toxins after acetaminophen (brand-name Tylenol) overdose, prolonged collapse of the circulatory system (shock) when the liver is deprived of fresh blood bringing oxygen and nutrients.
In this situation the AST and ALT serum levels can range anywhere from ten times the upper limits of normal to thousands of units/liter.
It’s rather hard to moderate elevations of the liver enzymes as they are often unexpectedly encountered on routine blood screening tests in otherwise healthy individuals. In such cases the AST and ALT levels are usually between twice the upper limits of normal and several hundred units/liter.
Fatty liver is one of the most common problems while moderating elevations of liver enzymes. In the United States, as in many other countries around the world, the most frequent causes of fatty liver are alcohol and drugs abuse, diabetes and obesity and sometimes chronic hepatitis C.
If you wish to know the aminotransferase level in your liver you should monitor and make some tests. It would be better if you pass complete test of AST (SGOT) and ALT (SGPT) levels, whether they are increasing, remaining stable, or decreasing. For example, patients undergoing treatment for chronic hepatitis C should be monitored with serial liver enzyme tests. Those ones responding to treatment will experience lowering of liver enzyme levels to normal or near normal levels. Those who develop relapse of hepatitis C after completion of treatment will usually develop abnormal liver enzyme levels again.
Alkaline phosphatase is an enzyme produced in the bile ducts, intestines, kidney, placenta and bone. When this enzyme level is high, and when ALT and AST levels are fairly normal, there may be a problem in the bile duct, such as an obstruction. Some bone disorders can also cause alkaline phosphatase levels to rise.
Elevation of alkaline phosphatase may indicate an injury to the biliary cells. Common causes of this are gallstones and certain mediations, although, some of the conditions listed previously can also raise the levels of this enzyme. Under physiological conditions, these enzymes are mainly allocated to the bile. In many pathological processes, a selection excretory enzyme in bile is disturbed, and their activity in blood plasma increases.
 Gamma-Glutamyltranspeptidase (GGT) enzyme, like alkaline phosphatase, is produced in the bile ducts and may become elevated when there is a bile duct disorder.
Gamma-Glutamyltranspeptidase (GGT) enzyme, like alkaline phosphatase, is produced in the bile ducts and may become elevated when there is a bile duct disorder.
High levels of GGT and AP hint at a possible blockage of the bile ducts, or of possible injury to, or inflammation of, the bile ducts. This type of problem is characterized by an impairment, or failure, of bile flow, which is known as cholestasis and refers to bile duct blockage or injury within the liver. As a rule, intrahepatic cholestasis occurs in people with primary biliary cirrhosis or liver cancer. Extrahepatic cholestasis refers to bile duct blockage or injury occurring outside the liver and may occur in people with gallstones.
GGT and AP can overflow like a backed up sewer and seep out of the liver and into the bloodstream but only in case of blockage or inflammation of the bile ducts. These liver enzymes are noticed approximately ten times the upper limit of normal.
When we talk about GGT we should mention that it is found predominantly in the liver, unlike AP which is mainly found in the bones but can also be found in many other organs, such as the intestines, kidneys, and placenta and of course liver. Taking into account, that GGT is a sensitive marker of alcohol ingestion and certain hepatotoxic (liver toxic) drugs it can be elevated without AP being elevated. It should be noted that for unclear reasons, people who smoke cigarettes appear to have higher AP and GGT than nonsmokers. Also, levels of AP and GGT are most accurate after a twelve-hour fast. You are beginning to get an inkling of the complexities that arise when evaluating abnormal LFTs!
The doctors determined that the normal level of AP ranges from 35 to 115 IU/L and normal level of GGT ranges from 3 to 60 IU/L. There are some causes of elevated AP and/or GGT:
- Alcoholic liver disease
- Primary biliary cirrhosis
- Liver tumors
- Primary sclerosing cholangitis
- Nonalcoholic fatty liver disease (NAFLD)
- Gallstones
- Drugs that are used for liver disease treatment
A new epidemiological study conducted over a ten-year period among more than 18 thousand specialists Mayo Clinic in Rochester, has determined that an excess amount of enzymes in the liver associated with the risk of death. High concentrations of aspartate aminotransferase and alanine aminotransferase in blood can not only to develop liver disease, but also cause a fatal outcome.
Doctors say that a simple blood test can identify those risks and prevent the subsequent death of the patient. According to American doctors, the availability of factors of hepatitis C and alcohol abuse may play a crucial role in shaping the preconditions for increased levels of enzymes. Also, researchers believe that the aspartate and alanine are markers of cardiovascular disease.
Total Bilirubin (TBIL)
The alkaline phosphatase and GGT levels are often elevated along with bilirubin in bile duct obstruction, or bile duct diseases.
The level of bilirubin in the blood can be elevated due to over-production, decreased uptake by the liver, decreased conjugation, decreased secretion from the liver or blockage of the bile ducts.
In such cases bilirubin can be elevated indirect and primarily. A lot of various liver diseases can cause elevated bilirubin levels.
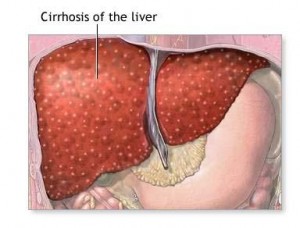
When the person suffers of chronic liver disease, here bilirubin levels are usually stable until a significant amount of liver damage has occurred and lead to cirrhosis. In acute liver disease, the bilirubin is usually increased relative to the severity of the acute process.
Albumin
Albumin is a very important protein for the liver. A little albumin leads to poor liver function. Commonly, the level of Albumin is normal in chronic liver diseases until cirrhosis and significant liver damage occur. If the person suffer of gastrointestinal and kidney disease, he may notice rather low albumin level.
Prothrombin Time (PT)
A type of blood clotting test performed in the laboratory and “prolonged” when the blood concentrations of some of the clotting factors made by the liver are low called prothrombin time. So, the synthesis and secretion of clotting proteins into the blood is decreased when liver function is severely abnormal.
If there is a non-cholestatic chronic liver disease, usually, the prothrombin time is not elevated until there cirrhosis or other liver damage occurring. All patients, which suffer of cholestatic liver disease can’t absorb vitamin K, which lead to prolonged prothrombin time. After patient’s recovering, the prothrombin time can be prolonged and return to normal.
Platelet Count
The platelet count can be abnormal in many conditions other than liver diseases, but in chronic liver diseases, it’s usually fall only after cirrhosis has developed.
Platelets are the smallest of the blood cells, which are involved in clotting. At the result of portal hypertension due to decreased blood flow through the liver because of scarring the spleen becomes enlarged and platelets can accumulate there.
Alpha Fetoprotein (AFP)
As a rule, for adults and children suffering chronic hepatitis B and C the doctors recommended to make special tests, in order to determine the level of alpha fetoprotein (AFP), which may show whether the person has some liver tumors or cancer. These tests are performed by ultrasound and AFP test every six months for risk category people, in order to detect and treat liver cancer, when it’s at the first stage.
When the Liver is diseased?
 Liver diseases can be divided into three groups. The first – focal disease, when struck by a station. It can be as tumors (benign and malignant), and cysts. Malignant tumors can grow both in the liver (if they are primary) or metastatic way. Carcinoma of the stomach, intestines, pancreas, usually go to the liver metastases. Cysts of the liver (the cavity containing the liquid) are parasitic (when the agent, for example, echinococcus) and no parasitic (congenital).
Liver diseases can be divided into three groups. The first – focal disease, when struck by a station. It can be as tumors (benign and malignant), and cysts. Malignant tumors can grow both in the liver (if they are primary) or metastatic way. Carcinoma of the stomach, intestines, pancreas, usually go to the liver metastases. Cysts of the liver (the cavity containing the liquid) are parasitic (when the agent, for example, echinococcus) and no parasitic (congenital).
The second group – diffuse liver disease. There is no single center; the disease spreads throughout the liver. These are acute hepatitis, which can go into chronic. And those in turn lead to cirrhosis and liver cancer.
The third group – diseases of the bile ducts. The most common cholelithiasis. While sometimes there is an inflammation of ducts, and even duct cancer.
Causes of focal, especially cancers, as a rule, are unknown. They are still learning. Benign cysts are congenital. The reason for stone formation is a metabolic disease. Hepatitis caused by viruses. And if three decades ago were known only two – A and B, then the doctors discovered a new group of viruses called hepatitis them “neither A – or B”. Began to study in detail – have opened hepatitis C. It is noteworthy that the hepatitis C virus has a number of genotypes, they are different.
Benign focal liver tumors, as a rule, are not dangerous for life. You can live with them. But only if you are confident in the diagnosis and if, for example, vascular tumor (hemangioma) – is a small size. If the tumors begin to grow in size, it can lead to abnormal liver function. Then it is better to remove them. Of course, a small benign cyst can be punctured. Parasitic cysts of the liver (Echinococcus) will inevitably grow, and they should be removed ass well as malignant tumors.
During the early stages of liver disease there are certain areas of the liver that may be prone to inflammation and scarring, including the lobules and the area where the large portal vein and its branches enter the liver, called the portal triad.
During the intermediate stages of liver disease, the fibrosis tissue or scarring expands and “bridges” between portal areas. Doctors assign “grades” to the degree of inflammation and liver cell damage and they identify “stages” of liver scarring and cirrhosis. These stages and grades are assessed as: none, minimal, mild, moderate or severe.
Warning! When liver disease is contraindicated:
- to receive hepatotoxic drugs (certain antibiotics and psychotropic drugs)
- physiotherapeutic procedures allowed after consultation with the doctor
- insolation (direct sunlight)
- vaccination (vaccine) – are allowed only after consultation with the doctor .
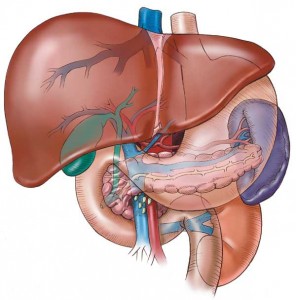
How does the Liver work?
The Liver is the biggest gland in the human’s body. It is about 2,5% of body weight, an average of 1.5 kg in men and 1.2 kg in women.
In general, the liver performs more than 500 different functions, participating in the regulation glucose (sugar) in the blood, accumulating nutrients – vitamins, iron, glycogen, producing bile to help break down fats.
But the main function of the liver is the barrier – cleansing. This is a powerful filter, neutralizing toxins which produced by metabolic reactions that converts toxic compounds, which removes and destroys the bacteria. It takes the blow in case of poisoning, drug overdoses and poor nutrition. The Liver rarely makes itself felt in the beginning of the disease. Usually, when there are symptoms, it has been already seriously ill.
Removal of this organ inevitably leads to death within 1-5 days. However, the liver has huge domestic reserves. It has the amazing ability to recover from injury, so the man can survive even after the removal of 70% of the liver tissue.
The liver produces a large number of liver enzymes entering directly into the blood. When liver is damaged some liver enzymes in the blood serum are decreased, while others – increased.